Abstract
Background: Following widespread exposure to Omicron variants, COVID-19 has transitioned to endemic circulation. Populations now have diverse infection and vaccination histories, resulting in heterogeneous immune landscapes. Careful consideration of vaccination is required through the post-Omicron phase of COVID-19 management to minimise disease burden. We assess the impact and cost-effectiveness of targeted COVID-19 vaccination strategies to support global vaccination recommendations.
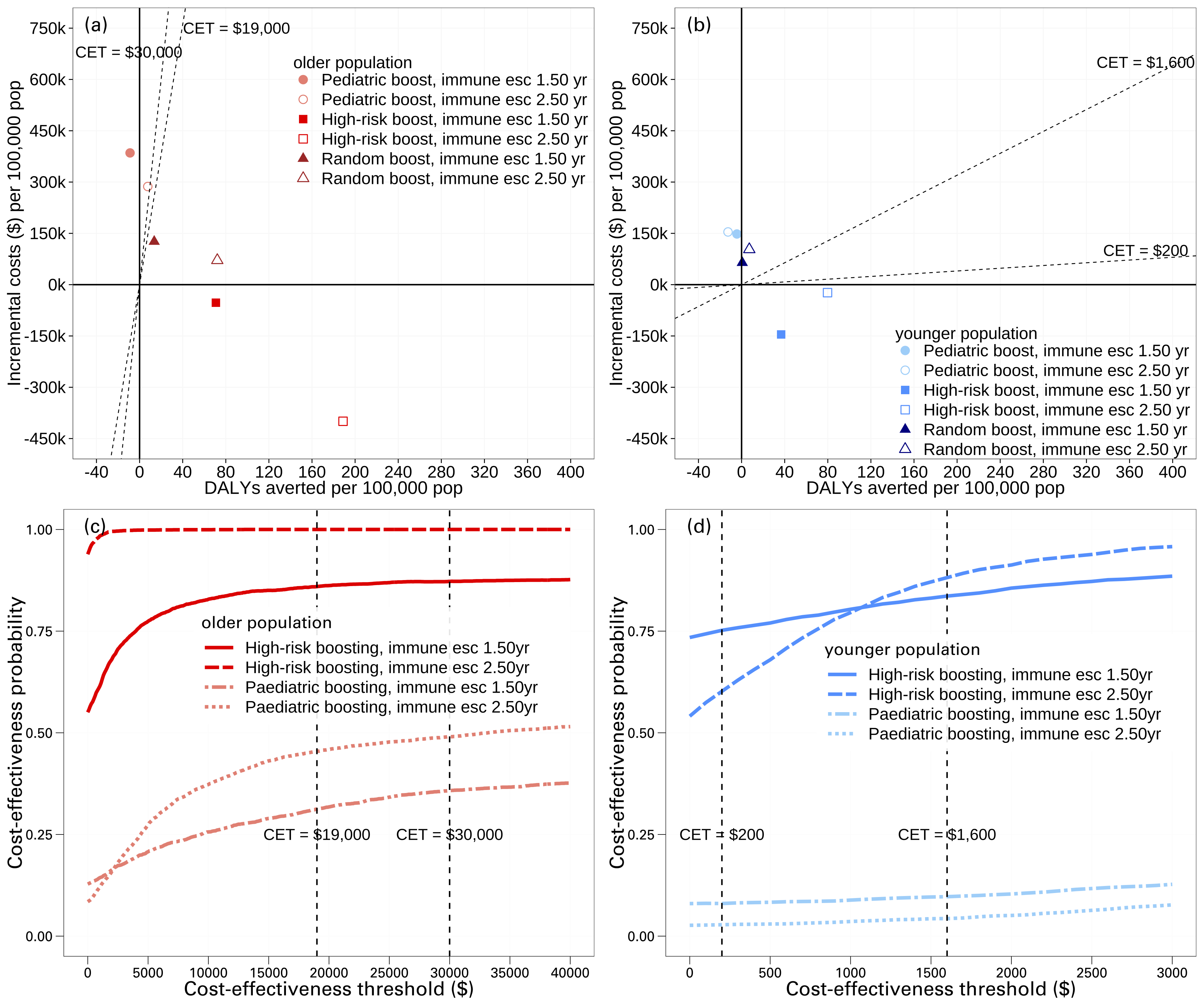
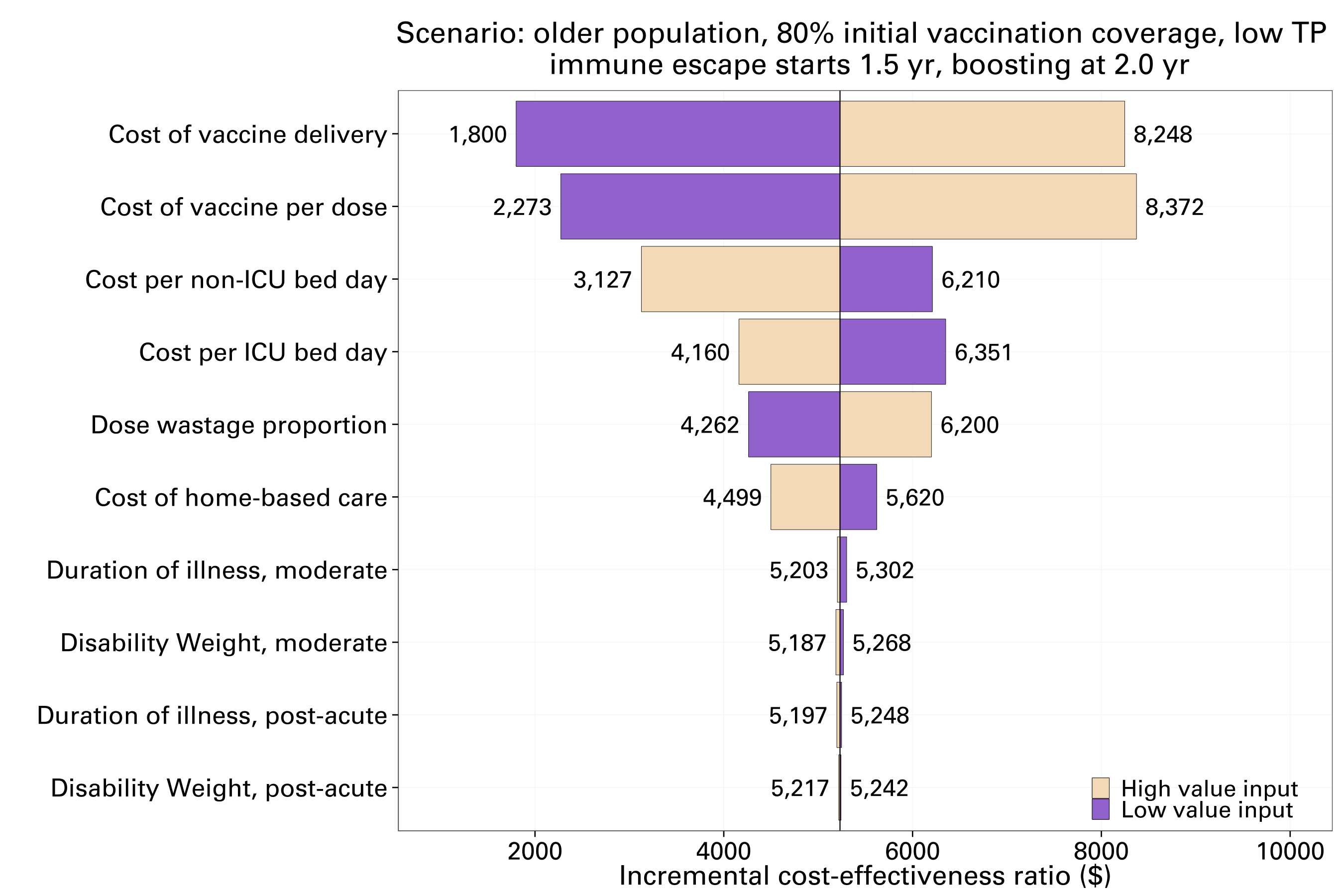
Methods: We integrated immunological, transmission, clinical and cost-effectiveness models, and simulated populations with different characteristics and immune landscapes. We calculated the expected number of infections, hospitalisations and deaths for different vaccine scenarios. Costs (from a healthcare perspective) were estimated for exemplar country income level groupings in the Western Pacific Region. Results are reported as incremental costs and disability-adjusted life years averted compared to no additional vaccination. Parameter and stochastic uncertainty were captured through scenario and sensitivity analysis.
Findings: Across different population demographics and income levels, we consistently found that annual elder-targeted boosting strategies are most likely to be cost-effective or cost-saving, while paediatric programs are unlikely to be cost-effective. Results remained consistent while accounting for uncertainties in the epidemiological and economic models. Half-yearly boosting may only be cost-effective in higher income settings with older population demographics and higher cost-effectiveness thresholds.
Interpretation: The seresults demonstrate the value of continued booster vaccinations to protect against severe COVID-19 disease outcomes across high and middle-income settings and show that the biggest health gains relative to vaccine costs are achieved by targeting older age-groups.
Figures